The name of our article is “How Autoimmune Diseases Cause Chronic Inflammation.” In this article, we discuss the relationship between food and chronic inflammation, particularly in relation to autoimmune diseases. We highlight the impact of changing one’s diet on chronic inflammation and provide strategies for incorporating an anti-inflammatory diet. Additionally, we mention the higher levels of inflammatory markers in individuals with fibromyalgia and emphasize the importance of consulting a doctor for medical advice and diagnosis. Overall, this article aims to inform readers about the connection between autoimmune diseases and chronic inflammation, as well as the potential role of diet in managing inflammation.
In the video titled “#066 Anti-inflammatory food diet for chronic inflammation, chronic pain, and arthritis” by Dr. Andrea Furlan, she delves into the relationship between the food we eat and pain. Chronic inflammation can lead to chronic pain, and there are certain nutrients in our Western diet that can increase inflammation. People with autoimmune diseases are more prone to inflammation due to their immune system attacking their own cells using inflammation. While it is unclear if fibromyalgia is an autoimmune disease, individuals with fibromyalgia tend to have higher levels of inflammatory markers. However, changing one’s diet can have a significant impact on chronic inflammation. Dr. Furlan provides strategies for incorporating an anti-inflammatory diet, such as avoiding refined carbohydrates and gluten, sugars and sweeteners, carbonated drinks, processed foods, trans fats and hydrogenated oils, red meat, alcohol, and excessive coffee. She also emphasizes the importance of consulting a doctor for medical advice and diagnosis.

This image is property of i.ytimg.com.
Autoimmune Diseases
Autoimmune diseases are a group of disorders characterized by the immune system’s abnormal response against the body’s own cells and tissues. This results in inflammation and damage to various organs and tissues. It is estimated that there are more than 80 different types of autoimmune diseases, affecting approximately 5-8% of the population worldwide. These diseases can range from mild to severe, and their symptoms can vary depending on the affected organs or tissues.
Some common autoimmune diseases include rheumatoid arthritis, lupus, multiple sclerosis, type 1 diabetes, celiac disease, and psoriasis. Each autoimmune disease has its own specific set of symptoms and can affect different parts of the body. For example, rheumatoid arthritis primarily affects the joints, while lupus can affect multiple organs including the skin, kidneys, and heart.
The exact cause of autoimmune diseases is still not fully understood. However, researchers believe that a combination of genetic and environmental factors play a role in their development. Genetic predisposition and certain triggering factors such as infections, hormonal changes, and exposure to certain drugs or chemicals can contribute to the onset of autoimmune diseases.
Chronic Inflammation
Inflammation is a natural immune response that helps the body fight off infections and heal injuries. However, when inflammation becomes chronic and persists for a long period of time, it can have detrimental effects on the body. Chronic inflammation is believed to be a key factor in the development and progression of various diseases, including autoimmune diseases.
Chronic inflammation is characterized by the prolonged activation of immune cells and the release of pro-inflammatory molecules called cytokines. This sustained immune response can damage healthy tissues and organs, leading to a range of symptoms and complications.
The mechanisms underlying chronic inflammation are complex and involve a variety of immune cells, signaling pathways, and inflammatory markers. Inflammation can be triggered by various factors, including infections, tissue damage, and exposure to toxins or allergens. In some cases, the immune system may become dysregulated and mistakenly target the body’s own cells and tissues, leading to autoimmune diseases.
Autoimmune Diseases and Chronic Inflammation
Autoimmune diseases and chronic inflammation are closely intertwined. In autoimmune diseases, the immune system mistakenly attacks the body’s own cells and tissues, leading to chronic activation of immune cells and the release of pro-inflammatory molecules. This sustained immune response contributes to the development of chronic inflammation.
The inflammatory response in autoimmune diseases involves the release of cytokines, such as tumor necrosis factor-alpha (TNF-alpha) and interleukins (IL-1, IL-6), and the activation of specific inflammatory pathways. These inflammatory molecules and pathways can lead to tissue damage and dysfunction in the affected organs.
The impact of chronic inflammation on target tissues and organs can be extensive. Inflammatory cells, such as macrophages and T cells, infiltrate the affected tissues and release toxic substances that cause damage. This can result in the destruction of healthy cells, impaired organ function, and the development of fibrosis or scar tissue.
Immune System Dysfunction in Autoimmune Diseases
The development of autoimmune diseases is often associated with immune system dysfunction. This dysfunction can manifest in several ways, including a lack of self-tolerance, immunosuppression failure, and abnormal activation of immune cells.
Lack of self-tolerance refers to the failure of the immune system to distinguish between self and non-self antigens. Normally, the immune system has mechanisms in place to prevent the attack on the body’s own cells and tissues. However, in autoimmune diseases, these mechanisms are faulty, leading to the immune system mistakenly targeting self antigens.
Immunosuppression failure occurs when the mechanisms that regulate or suppress immune responses are ineffective. This can result in the overactivation of immune cells and the sustained release of pro-inflammatory molecules, contributing to chronic inflammation.
Abnormal activation of immune cells, such as T cells and B cells, is also observed in autoimmune diseases. These cells become hyperresponsive to antigens and exhibit abnormal behaviors, leading to the production of autoantibodies and the destruction of healthy cells.
Inflammatory Response in Autoimmune Diseases
The inflammatory response in autoimmune diseases is characterized by the release of pro-inflammatory cytokines, activation of inflammatory pathways, and recruitment of immune cells to target sites.
Pro-inflammatory cytokines, such as TNF-alpha, IL-1, and IL-6, play a crucial role in initiating and sustaining inflammation. These cytokines promote the activation of immune cells, increase vascular permeability, and attract inflammatory cells to the site of inflammation.
Inflammatory pathways, such as the nuclear factor-kappa B (NF-kB) pathway and the Janus kinase-signal transducer and activator of transcription (JAK-STAT) pathway, are activated in autoimmune diseases. These pathways amplify the inflammatory response and regulate the production of inflammatory molecules.
Recruitment of immune cells, such as neutrophils, macrophages, and T cells, to the target sites of inflammation is essential for tissue damage and destruction. These immune cells release toxic substances, phagocytose damaged cells, and promote further inflammation, contributing to the progression of autoimmune diseases.
Impact on Target Tissues and Organs
The chronic inflammation associated with autoimmune diseases can have significant impacts on target tissues and organs.
Tissue damage and destruction occur as a result of sustained inflammation and the release of toxic substances by immune cells. This can lead to the breakdown of healthy cells, disruption of tissue architecture, and the formation of scar tissue. Over time, tissue damage can impair organ function and contribute to the development of chronic complications.
The impaired function of affected organs is a common consequence of chronic inflammation in autoimmune diseases. For example, in rheumatoid arthritis, chronic inflammation in the joints can cause pain, swelling, and stiffness, leading to reduced mobility and disability. In autoimmune hepatitis, chronic inflammation in the liver can disrupt its normal function, potentially leading to cirrhosis and liver failure.
The development of chronic inflammation in autoimmune diseases can perpetuate a cycle of tissue damage and ongoing inflammation. The continuous release of pro-inflammatory molecules and the recruitment of immune cells to target sites sustain the inflammatory response, leading to a chronic state of inflammation.
Link Between Autoimmune Diseases and Fibromyalgia
Fibromyalgia is a chronic pain condition characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances. While the exact cause of fibromyalgia is unknown, there is evidence to suggest a link between autoimmune diseases and fibromyalgia.
Studies have shown that people with fibromyalgia have higher levels of inflammatory markers compared to those without fibromyalgia. These inflammatory markers, such as C-reactive protein and pro-inflammatory cytokines, indicate the presence of chronic inflammation in the body. This suggests that chronic inflammation may play a role in the development and progression of fibromyalgia.
The mechanisms of interaction between autoimmune diseases and fibromyalgia are not fully understood. However, it is hypothesized that the underlying autoimmune processes and chronic inflammation in autoimmune diseases may contribute to the development or worsening of symptoms in fibromyalgia. Further research is needed to fully elucidate this relationship.
The Role of Diet in Chronic Inflammation
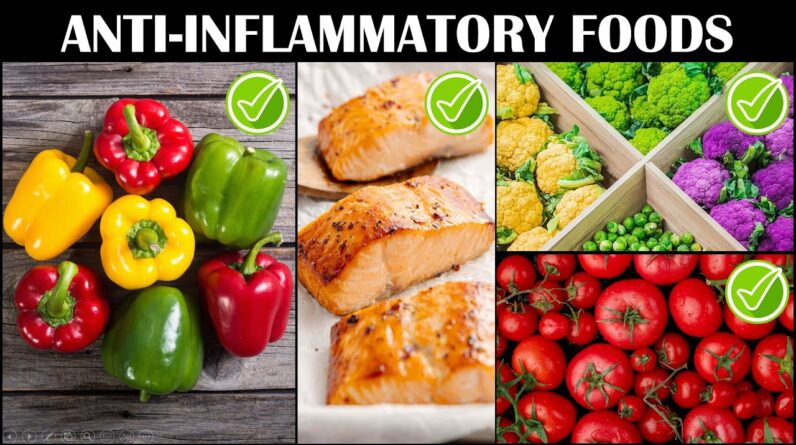
Diet plays a crucial role in chronic inflammation, and making dietary changes can have a significant impact on reducing inflammation and improving overall health. An anti-inflammatory diet focuses on consuming foods that have anti-inflammatory properties and avoiding foods that promote inflammation.
The key principles of an anti-inflammatory diet include:
-
Avoiding refined carbohydrates and gluten: Refined carbohydrates, such as white bread, pasta, and pastries, can spike blood sugar levels and promote inflammation. Gluten, found in wheat and other grains, can also trigger inflammation in some individuals with gluten sensitivities or autoimmune diseases like celiac disease.
-
Eliminating sugars and sweeteners: Excessive sugar consumption can lead to chronic inflammation and various health issues. Artificial sweeteners such as aspartame and sucralose have also been associated with increased inflammation. Opt for natural sweeteners like honey or maple syrup in moderation.
-
Cutting out carbonated drinks: Soda and other carbonated beverages contain high amounts of sugar and artificial additives, which can contribute to inflammation. Replace these drinks with water, herbal teas, or freshly squeezed juices.
-
Avoiding processed foods: Processed foods often contain unhealthy fats, high levels of sodium, and artificial additives, all of which can promote inflammation. Opt for whole, unprocessed foods like fruits, vegetables, lean proteins, and whole grains.
-
Eliminating trans fats and hydrogenated oils: Trans fats, found in fried foods, margarine, and many packaged snacks, are highly inflammatory. Hydrogenated oils, often used in processed foods, can also contribute to inflammation. Cook with healthier oils like olive oil and consume foods with natural fats like avocados and nuts.
-
Reducing red meat consumption: Red meat is high in saturated fats and can promote inflammation when consumed in excess. Limit your intake of red meats and opt for leaner protein sources like fish, poultry, or plant-based proteins.
-
Limiting alcohol and excessive coffee: Alcohol and excessive coffee consumption can lead to inflammation and may worsen symptoms in autoimmune diseases and fibromyalgia. Moderation is key, and it’s advisable to limit alcohol to one drink per day and coffee to 1-2 cups.
-
Avoiding packaged snacks: Packaged snacks often contain unhealthy fats, refined carbohydrates, and artificial additives that can promote inflammation. Instead, opt for homemade snacks like fruits, nuts, or yogurt.
It’s important to note that individual dietary needs may vary, and consulting a doctor or registered dietitian is advisable for personalized advice and guidance.
Strategies for Incorporating an Anti-Inflammatory Diet
Incorporating an anti-inflammatory diet into your lifestyle can be a gradual process. Here are some strategies to help you adopt healthier eating habits:
-
Avoiding refined carbohydrates and gluten: Replace white bread and pasta with whole grain options like quinoa, brown rice, or buckwheat. Experiment with gluten-free alternatives for bread, pasta, and baked goods.
-
Eliminating sugars and sweeteners: Gradually reduce your intake of sugary desserts, soda, and sweetened beverages. Opt for naturally sweetened options like fresh fruits or homemade treats sweetened with natural sweeteners.
-
Cutting out carbonated drinks: Substitute soda and carbonated drinks with water, herbal teas, infused water, or freshly squeezed juices. Add slices of citrus fruits or berries to enhance the flavor.
-
Avoiding processed foods: Choose fresh, whole foods whenever possible. Cook at home using fresh ingredients and minimize your consumption of pre-packaged meals, snacks, and fast food.
-
Eliminating trans fats and hydrogenated oils: Read food labels and avoid products that contain trans fats or hydrogenated oils. Cook with healthier oils like olive oil, avocado oil, or coconut oil.
-
Reducing red meat consumption: Incorporate plant-based proteins like beans, lentils, tofu, or tempeh into your meals. Limit red meat consumption to once or twice a week and choose lean cuts.
-
Limiting alcohol and excessive coffee: Moderation is key. Limit your alcohol intake to one drink per day for women and up to two drinks per day for men. Limit your coffee consumption to 1-2 cups per day.
-
Avoiding packaged snacks: Instead of reaching for packaged snacks, include whole foods in your snack choices. Choose fresh fruits, vegetables with hummus, nuts, or homemade energy bars.
It’s important to note that an anti-inflammatory diet is just one aspect of managing chronic inflammation and autoimmune diseases. Other lifestyle factors such as regular exercise, stress management, and getting enough sleep are also important for overall health and well-being.
Consulting a doctor or registered dietitian is recommended for personalized advice, especially if you have specific dietary restrictions or medical conditions.
Conclusion
Autoimmune diseases and chronic inflammation are closely interconnected, with chronic inflammation playing a significant role in the development and progression of autoimmune diseases. Managing inflammation is crucial for individuals with autoimmune diseases and fibromyalgia, as it can impact their symptoms and overall health.
Incorporating an anti-inflammatory diet can be a valuable complementary approach to managing chronic inflammation. By avoiding foods that promote inflammation and consuming those with anti-inflammatory properties, individuals can potentially reduce inflammation and improve their overall well-being. However, it’s important to remember that diet alone may not be sufficient, and a comprehensive approach that includes medical treatment, lifestyle modifications, and professional guidance is essential for optimal management.
Seeking professional advice from a doctor or registered dietitian is crucial to ensure that any dietary changes align with individual needs and health conditions. With the right strategies and support, individuals with autoimmune diseases and chronic inflammation can take proactive steps towards managing their condition and improving their quality of life.